Painful bladder symptoms, also known as bladder pain syndrome or interstitial cystitis, can be a debilitating condition for women. The condition is characterized by chronic pelvic pain, urinary urgency and frequency, and discomfort during sexual intercourse. Painful bladder symptoms can significantly impact a woman’s quality of life, making it difficult to work, exercise, and engage in social activities. This blog will discuss the causes of painful bladder symptoms in women, how it is diagnosed and treated, and ways to manage the condition to improve quality of life.
Causes of Painful Bladder Symptoms in Women:
The exact cause of painful bladder syndrome is not well understood. However, researchers have identified a few potential contributing factors to the condition. Some of these factors include:
- Defects in the bladder lining: Research suggests that people with painful bladder symptoms may have a defect in the bladder lining that makes it more susceptible to irritation and damage.
- Autoimmune disorders: Some women with painful bladder symptoms may have an autoimmune disorder that causes their immune system to attack the bladder lining, leading to inflammation and pain.
- Chronic infection: Chronic bladder infections or urinary tract infections (UTIs) can cause damage to the bladder lining and trigger painful bladder symptoms.
- Neurological conditions: Some neurological conditions, such as multiple sclerosis or spinal cord injuries, can damage the nerves that control bladder function, leading to painful bladder symptoms.
Diagnosing Painful Bladder Symptoms:
Diagnosing painful bladder syndrome can be challenging because there is no specific test or diagnostic tool available to confirm the condition. Doctors usually diagnose the condition based on a person’s symptoms and ruling out other possible conditions. Some of the tests that doctors may use to diagnose painful bladder syndrome include:
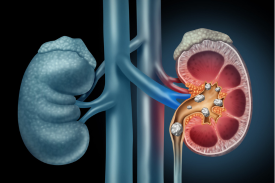
- Urine analysis: A urine test can help to rule out a urinary tract infection or other conditions that may cause similar symptoms.
- Cystoscopy: A cystoscopy involves inserting a small camera into the bladder to look for signs of inflammation, damage, or other abnormalities.
- Biopsy: In some cases, a doctor may take a small tissue sample from the bladder lining to look for signs of inflammation or other abnormalities.
- Urodynamics testing: Urodynamics testing measures the pressure in the bladder during urination to help identify any problems with bladder function.
Treating Painful Bladder Symptoms:
Treatment for painful bladder syndrome aims to reduce symptoms and improve a person’s quality of life. Some of the treatment options for the condition include:
- Medications: Medications can help to reduce inflammation and pain associated with painful bladder syndrome. Some of the medications that may be used to treat the condition include nonsteroidal anti-inflammatory drugs (NSAIDs), tricyclic antidepressants, and antihistamines.
- Bladder instillations: Bladder instillations involve inserting a liquid medication directly into the bladder through a catheter. The medication helps to reduce inflammation and pain in the bladder lining.
- Physical therapy: Physical therapy can help to strengthen the pelvic floor muscles and improve bladder function. Some women with painful bladder syndrome may benefit from pelvic floor muscle exercises or biofeedback training.
- Nerve stimulation: Nerve stimulation involves using a small electrical device to stimulate the nerves that control bladder function. This can help to reduce bladder spasms and improve bladder control.
- Surgery: In rare cases, surgery may be necessary to treat painful bladder syndrome. Surgical options may include bladder augmentation or removal of the bladder.
In addition to medical treatments, there are several ways women can manage their painful bladder symptoms to improve their quality of life. Here are some strategies to consider:
- Dietary modifications: Certain foods and beverages, such as caffeine, alcohol, and spicy foods, can exacerbate painful bladder symptoms. Keeping a food diary to track which foods trigger symptoms can help identify dietary triggers. It may be helpful to limit or avoid these foods altogether.
- Stress reduction: Stress can worsen painful bladder symptoms. Engaging in stress-reducing activities such as meditation, deep breathing, or yoga can help manage stress levels.
- Bladder retraining: Bladder retraining involves gradually increasing the time between trips to the bathroom to train the bladder to hold more urine. This can help reduce urinary frequency and urgency.
- Pelvic floor exercises: Strengthening the pelvic floor muscles can help improve bladder control and reduce urinary urgency and frequency. Women can work with a physical therapist to learn pelvic floor exercises or use a pelvic floor exercise device.
- Avoiding bladder irritants: Certain chemicals, such as perfumes, dyes, and other irritants, can trigger painful bladder symptoms. Avoiding these irritants can help manage symptoms.
- Heat therapy: Applying a heating pad or warm compress to the lower abdomen can help reduce pelvic pain and discomfort associated with painful bladder syndrome.
- Support groups: Joining a support group or speaking with others who have similar experiences can help women feel less isolated and provide emotional support.
It’s essential to work with a healthcare provider to develop an individualized treatment plan that addresses a person’s unique symptoms and needs.
Conclusion:
Painful bladder syndrome can significantly impact a woman’s quality of life, but there are ways to manage the condition to improve symptoms and reduce discomfort. The causes of painful bladder syndrome are not entirely understood, making it challenging to diagnose and treat. However, working with a healthcare provider to develop a personalized treatment plan that addresses a person’s unique symptoms and needs can be effective in managing the condition. Additionally, making lifestyle modifications, such as dietary changes, stress reduction, and pelvic floor exercises, can help manage symptoms and improve quality of life. With proper management, women with painful bladder syndrome can lead healthy, fulfilling lives.